- Undergraduate
Bachelor's Degrees
Bachelor of ArtsBachelor of EngineeringDual-Degree ProgramUndergraduate AdmissionsUndergraduate Experience
- Graduate
Graduate Experience
- Research
- Entrepreneurship
- Community
- About
-
Search
All Thayer News

Tissue Engineers Work to Improve Quality of Life for Cancer Patients
Sep 11, 2024 | DH-Geisel Giving
Cancer treatment can save a patient's life, but it often leaves substantial damage in its wake. When surgeons remove cancerous tumors, they frequently take out significant portions of adjacent tissue and bone. This can alter a patient's appearance and impair bodily functions, affecting their physical and mental well-being during recovery.

Professor Hixon discusses printing methods and material choice for bone healing with Peter Bertone, surgical PhD Innovation Program candidate, in the process of UV-curing 3D-printed scaffolds. (Photo by Rob Strong '04)
Now, tissue engineers at Dartmouth are developing methods to repair, rehabilitate, and replace such damaged tissue. Their work, led by Dartmouth Engineering professor Katie Hixon, who is also clinical assistant professor of orthopedics at Geisel School of Medicine, aims to improve the quality of life for patients after cancer treatment.
Hixon's research has been supported by the Dartmouth Innovations Accelerator for Cancer (DIAC), a philanthropic initiative that provides essential funding and entrepreneurial training for innovative cancer-related projects. Established by the Geisel School of Medicine in partnership with the Magnuson Center for Entrepreneurship at Dartmouth in partnership with the Dartmouth Cancer Center, DIAC aims to commercialize innovations and connect researchers with potential investors.
"Tissue engineered scaffolds serve as vehicles," Hixon says of the importance of maintaining healthy tissue in cancer patients. "With them, you can deliver chemotherapies, help the tissue to repair after radiation, or even modify the immune response."
Together with her team of graduate, undergraduate, and medical students, Hixon uses cell therapies, biomaterial scaffolds, and growth factor delivery systems to create customized, living tissue constructs. Implanting a tissue engineering "scaffold" allows surgeons to restore, improve, and replace the damaged tissue.
The implant Hixon creates helps the body heal itself, she explains. "Then it degrades over time as the tissue replaces it, attracting the right types of cells, blood vessels, and other components for healthy tissue regeneration."
These living tissue scaffolds are usually tailored to address precise needs for patients as they navigate the aftermath of lifesaving but invasive treatments. "Our scaffolds are easy to tailor to the pathology we're working with," says Hixon. "Which is important with cancer, because there are so many kinds of cancer, and cancer targets different ages and body types. So, our scaffolds have that tunability. They're very adaptable."
Tissue engineering offers immense remedial promise after surgery, often accelerating recuperation. After surgery, the bone is usually very weak, prone to infection and fracture. "Putting our scaffolds in helps the healthy bone to grow back," Hixon notes. "Ideally, our scaffold strengthens the site of injury. This can be very helpful in the context of metastatic bone disease, which is often very painful in various aspects."
Hixon's foray into the relatively new field of tissue engineering began with bone reconstruction research, primarily following traumatic injuries. But soon after coming to Dartmouth in 2022, she began to apply her expertise to help cancer patients post-surgery, noting that they often experience a traumatic injury when surgeons removed metastatic, primary, or other tumors.
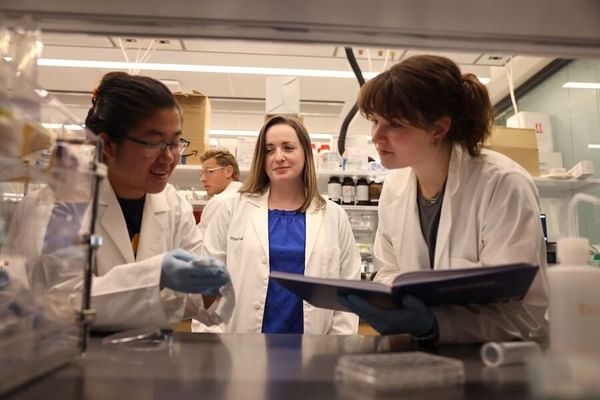
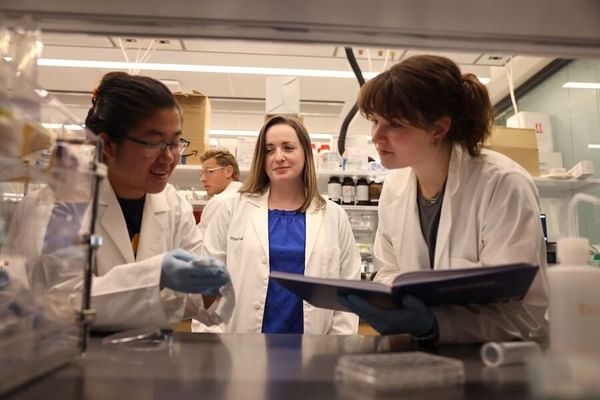
Hixon observes as Michelle Tong, summer intern, and Adelaide Cagle, surgical PhD Innovation Program candidate, collaborate on their electrospun scaffold for dermal tissue engineering in their lab at the Engineering and Computer Science Center at Dartmouth. (Photo by Rob Strong '04)
"I had never really explored the cancer space before," Hixon says matter-of-factly, adding that she has had a lot of help. Hixon credits much of her lab's success to her talented team of graduate and undergraduate students. "The students really ran with it."
Hixon's work has been bolstered by substantial support from DIAC. In March 2022, her team was awarded $50,000 as part of DIAC's Third Cohort 5-Week Track. Later that year, in December, they received an additional $25,000 Stu Trembly Award. Most recently, in December 2023, Hixon's team was awarded another $15,000 Stu Trembly Award as part of DIAC's Fourth Cohort. This funding, totaling $90,000, has been instrumental in advancing her research from the laboratory to animal models and closer to real-world applications.
Hixon and her team began creating scaffolds for cancer patients by working with cells and biomaterials in the laboratory. For the scaffolds to be useful in the real world, however, she needed to see how they would respond to cancer radiation. Normally, her scaffolds promote healing and bone growth. But after a tumor is removed, patients often undergo radiation, which "is very harmful to tissue and prevents new bone from forming or forming very well."
Hixon and her team thus needed to study how a scaffold might behave after being implanted into a patient undergoing treatment. To do that, they turned to animal models, made possible by critical support from DIAC.
For Hixon, DIAC supporting this transition from the lab to living tissues has made all the difference. "It really takes it to another level when you're working with living models as opposed to just working with cells in the lab," she says. Her animal model research explores whether the scaffolds "bypass inappropriate or insufficient bone formation and lead to proper healing." If so, this could be very promising for human patients.
For example, consider a patient with osteosarcoma who undergoes surgery to remove a tumor from the femur, resulting in a significant bone defect. Scaffolding technology could potentially regenerate the lost bone, restoring structural integrity and functionality. While still in development, this approach illustrates the transformative potential of this research for bone cancer survivors, helping them regain mobility and independence after treatment and reducing the risk of amputation. This innovation offers hope for a future where patients can return to normal activities and feel whole again.
In addition to facilitating important research, DIAC has helped bridge Hixon's background in academia with the business acumen needed to turn her innovations into real-world impact. While students and residents assist with surgeries and longitudinal analysis of research data, the lab team also works with students in Dartmouth's Tuck School of Business to move research further down the accelerator pipeline. Bringing the Hixon Lab's scientific innovations closer to widespread adoption has "really been a team effort," she says.
Next, Hixon has her sights set on advancing bioengineered solutions for craniofacial reconstruction. "In the future, we want to move to more complex structures and geometry, such as tumors in the jaw, which is much more complicated because your face is so intricate and important in how we communicate," she says. "That's something we're all really passionate about—helping people to feel like themselves again."
Hixon Lab member Peter Bertone was the winner of the 2024 Orthopaedic Research Society (ORS) International Section Fracture Repair (ISFR) 3-Minute Research Pitch Competition.
For contacts and other media information visit our Media Resources page.
