- Undergraduate
Bachelor's Degrees
Bachelor of ArtsBachelor of EngineeringDual-Degree ProgramUndergraduate AdmissionsUndergraduate Experience
- Graduate
Graduate Experience
- Research
- Entrepreneurship
- Community
- About
-
Search
All Thayer News


Dartmouth Researchers File Patent for Device to Advance Breast Cancer Detection and Monitoring
May 10, 2023 | by Catha Mayor
A team of four researchers from Dartmouth Engineering and Dartmouth Hitchcock Medical Center (DHMC) has filed a patent for a customizable optical breast imaging device designed to significantly improve both breast cancer diagnosis and treatment monitoring.

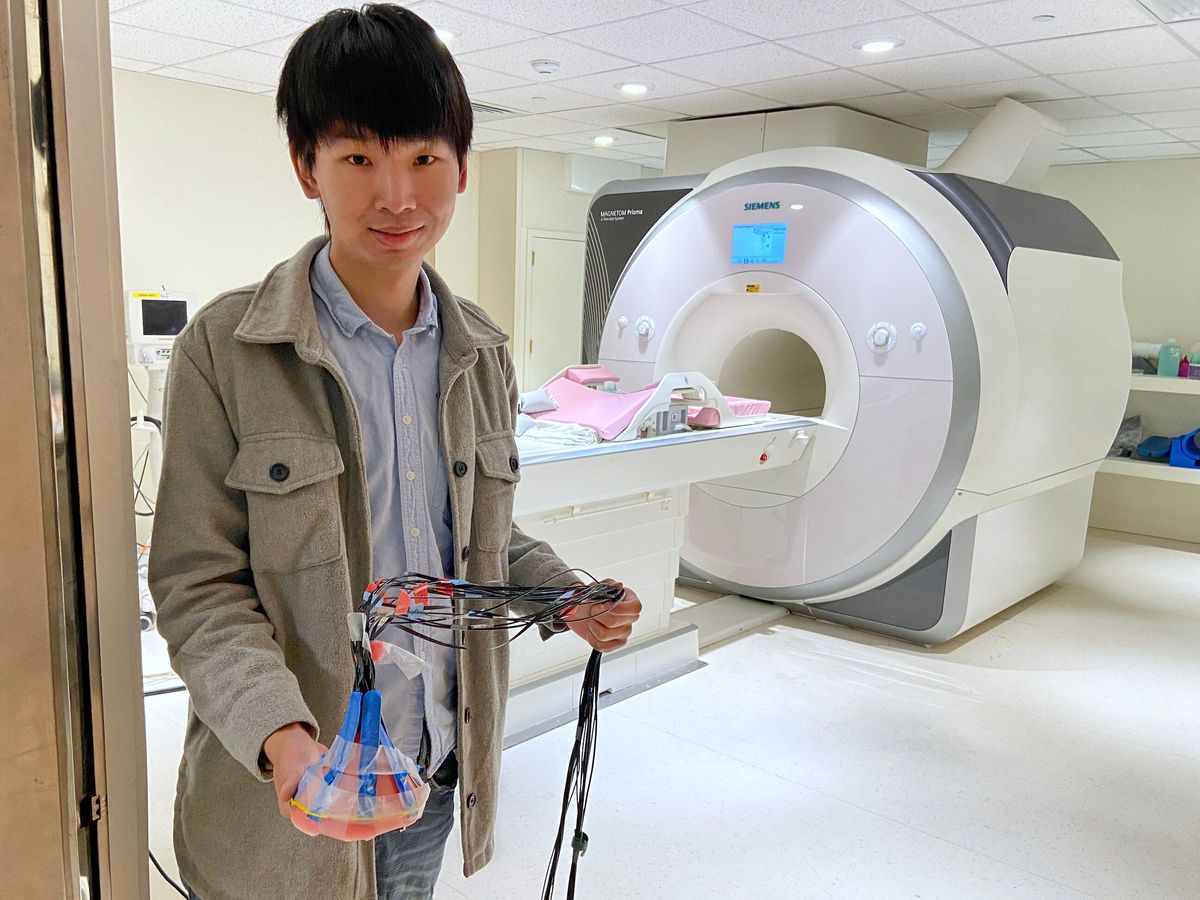
The research team (l to r): Robert A. Pritzker Professor of Biomedical Engineering Keith Paulsen, engineering PhD student Mengyang Zhao, Professor of Engineering Shudong Jiang, and DHMC MRI Technologist Shreve Soule. (Photo by Catha Mayor)
The device can be used either inside a magnetic resonance imaging (MRI) scanner to obtain both MRI and near-infrared spectral tomography (NIRST) scans simultaneously, or on its own to monitor tumor response to chemotherapy. It has potential to be used for not only breast imaging but also other applications such as muscle and brain function imaging.
Professor of Engineering Shudong Jiang has been working with Robert A. Pritzker Professor of Biomedical Engineering Keith Paulsen, as well as PhD student Mengyang Zhao and MRI Technologist Shreve Soule, to develop and refine the device. We spoke with Professor Jiang about what she describes as, "my major work."
What problem were you trying to solve with this device?
The Optics in Medicine group has been working for over fifteen years to improve the accuracy, sensitivity, and specificity of breast cancer imaging and diagnosis. Contrast MRI is the current gold-standard, but for that you need to inject a contrast agent which can cause side effects and increases imaging time and costs. If you use MRI without a contrast agent, the problem is the specificity. You may know something's there but you don't know if it's cancer or benign. What we've done is combine optical imaging with MRI to improve diagnostic performance without side effects.
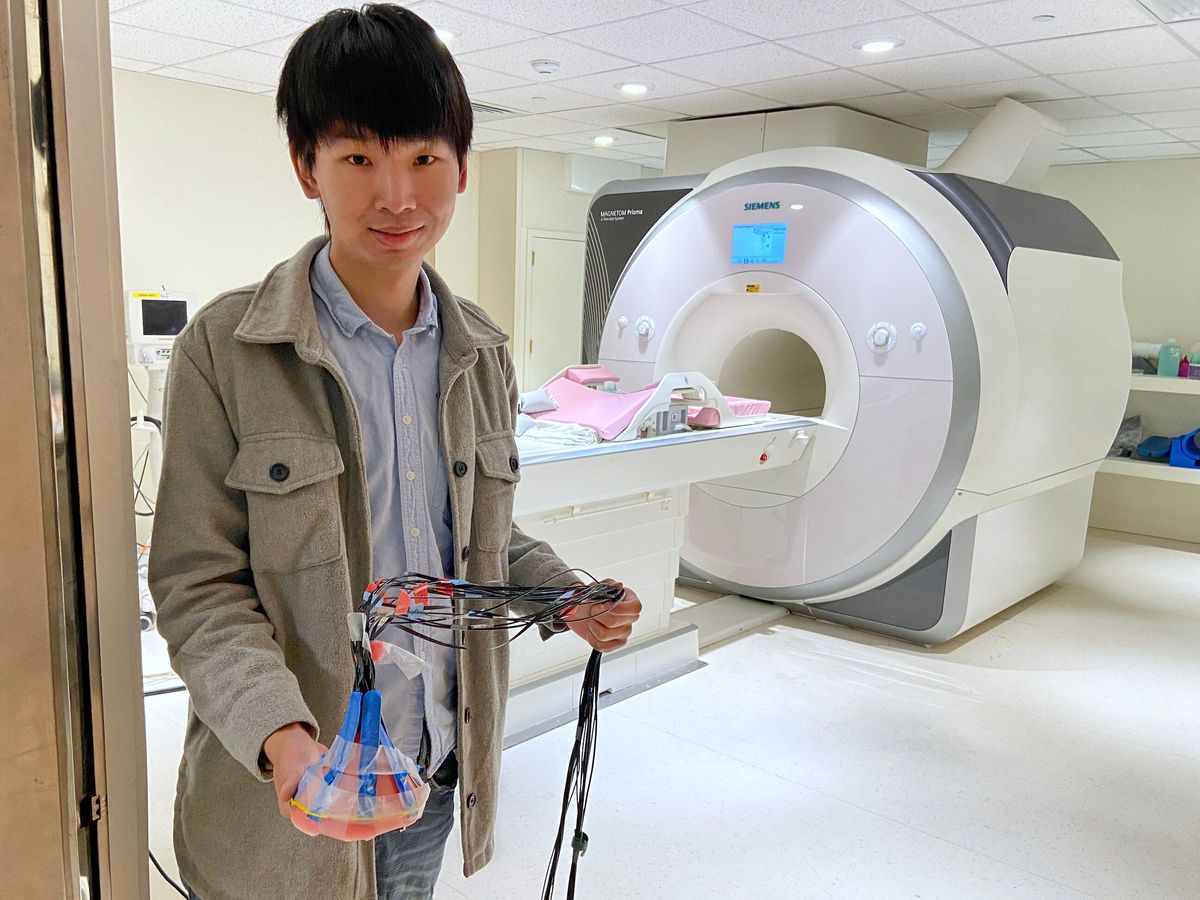
Engineering PhD student Mengyang Zhao preps the NIRST system for testing in the MRI scanner at DHMC. (Photo by Catha Mayor)
How does it work?
Our device uses a set of flexible optoelectronic strips as part of a specialized NIRST system. NIRST can provide tissue metabolism and vascular characteristics, but the spatial resolution is not high enough to detect early-stage breast cancer. So we developed a system to obtain both MRI and NIRST images simultaneously. Sixteen MRI-compatible optical fibers are attached to the MRI breast coil through an adjustable NIRST interface, for light delivery and collection. This type of MRI-guided NIRST can significantly improve diagnostic performance for breast cancer.
What design challenges did you have to overcome?
Our first design got really good results without the contrast agent. We could clearly distinguish cancer from benign tissue, but it used huge, bulky fiber bundles. It was awkward and heavy and difficult to cover the whole breast. It also took hours to reconstruct the images with computer models.
So we decided to develop a different design. We integrated our detectors and fibers into a flexible plastic strip that can fit the breast shape and get full coverage no matter where the tumor is. And now we use deep learning methods to obtain the images in seconds.
For the deep learning methods, we've been able to train the computer using simulated patient data sets based on typical locations, shapes, and properties of tumors. With our knowledge about how breast cancer typically presents, we were able to generate more than 20,000 data sets to train the computer in breast cancer detection. We also use a similar method to monitor cancer treatment.

Professor Jiang works with PhD student Zhao to analyze and evaluate the system's performance. (Photo by Catha Mayor)
How does it work to monitor tumor response to chemotherapy?
We use the same NIRST system on its own to be able to watch tumor response to early-stage chemo. If the tumor isn't responding, then doctors can stop the chemo and adjust the medicine or switch to surgery right away instead of waiting four to six months to complete the full treatment and then discover it wasn't effective.
Originally, we made the device for breast cancer detection inside of an MRI. That's more difficult because you can't use any metal and the wires require a special design. But for the chemo monitoring, that's much easier.
Switching from the huge fiber bundles, not only is the image quality much better, but also the system is faster and more compact, which is important for this application. We need to be able to easily transport it to the infusion unit, and then take five minutes or less to image the patient before the first infusion starts. Then we image again before the second infusion to determine if the treatment is effective.
What was the hardest part of the development process?
We had a lot of trouble finding a company to make the device for us and go through the needed iterations. We started designing at the beginning of 2020 and finally got the first one made in 2021. It was difficult. We would wait for weeks, then finally get one in the mail and it would be completely wrong, or too rough. And then we would want to switch to a different type of fiber or detector and that would take months.
For use in the MRI, at first we didn't pay enough attention to the design of the wires and it turned out to be a burn hazard for the patients. We needed guidance from an MRI expert. So I asked a former student of Keith Paulsen's named Alex Lee, who now has a high-level position at one of the largest MRI companies in the world.
I called him and said, "I really need your help." He introduced me to a specialist who worked with us to troubleshoot our design. We had two wires for grounds, but the strong magnetic field was causing a high current in the loops of these grounds. The specialist taught us that when you layout the wire cables, you can't do any loops.
If he didn't tell me, I never would have thought the two grounds would cause a problem! So we finally got the full working prototype last summer and were able to file for the patent.
What's next for this project?
The next step is to test the system with breast cancer patients to determine exactly how efficient it is at detecting breast cancer when combined with MRI. At the same time, we will continue work on making the device even faster, more compact, and more convenient for monitoring and predicting treatment response, as well as exploring new clinical applications for this unique imaging system.
For contacts and other media information visit our Media Resources page.
